Why Does America Have Fewer Types of IUDs Than Other Countries?
The land of choice has more limited options when it comes to contraception.
My uterus needs more options. In 2013, a gynecologist told me that it was too short to fit any FDA-approved IUD. So I traipsed from Colorado to Canada to get a smaller IUD called the GyneFix. This IUD isn’t shaped like a “T”—as all American IUDs are—but, rather, a rod.
Three years later, my now-ex-gynecologist saw the copper rod in an ultrasound. He assumed that, because he couldn’t see them, the IUD’s T-shaped arms must be embedded in the walls of my uterus. We decided on surgery to remove it. Somehow I’d forgotten that this particular IUD didn’t have arms.
The surgery took two hours. He inserted a light and camera through my belly button, like that robotic worm in the Matrix. Then he made a hole near my left hip to find these phantom IUD arms with a tweezer-scissor tool called graspers.
“I couldn’t find the arms,” he told me, puzzled, when I woke up from anesthesia. It must have been frustrating to hunt for something for so long that didn’t exist. After he left, I looked under the hospital blanket at his two neat incisions. Underneath, my flesh tried to pull itself together.
Since my gyno later insisted that the GyneFix had still been embedded, even once he admitted it didn’t have arms, I decided the pill was my next best option. Within a year I realized it was making my hair fall out, a rare side effect, and stopped taking it. Because all hormonal birth controls use the same hormones, I couldn’t use any if I wanted to keep my hair. My choices dwindled to barrier methods like condoms, which work just 77 percent of the time.
So I emailed Dirk Wildemeersch, the Belgian gynecologist who invented the GyneFix. I attached my ultrasound records and asked if it had actually been embedded in my uterus. The IUD was completely within my uterine cavity, he replied, and not at all embedded. Wildemeersch told me that I’m still a good candidate for the GyneFix, and I could visit his clinic in Belgium to get another. Canada was no longer an option because I’d been part of a clinical trial that had since ended, and the GyneFix isn’t yet commercially approved there.
One in 15 women have a uterine abnormality, which typically affects the walls and shape of the uterus. And even “normal” uteruses are different. “Individual variations in the size and shape of the human uterus are probably greater than variations in the size and shape of the human foot,” wrote the late OB/GYN Harrith Hasson, who invented the surgery that removed my GyneFix. For instance, uterine widths range from less than 10 millimeters to more than 50. Women who haven’t given birth average 27—a millimeter smaller than the narrowest IUD available in America, the Skyla. Women can use IUDs that are wider than their uterus, but they come with a higher risk of side effects like failed and difficult fittings, pain, abnormal bleeding, expulsion, embedment, and pregnancy. Just 30 percent of women who haven’t given birth opt to keep in a standard 32-millimeter width copper IUD, such as the ParaGard, after one year. By contrast, 70 to 90 percent stick with narrower IUDs or rods like the GyneFix even after three years.
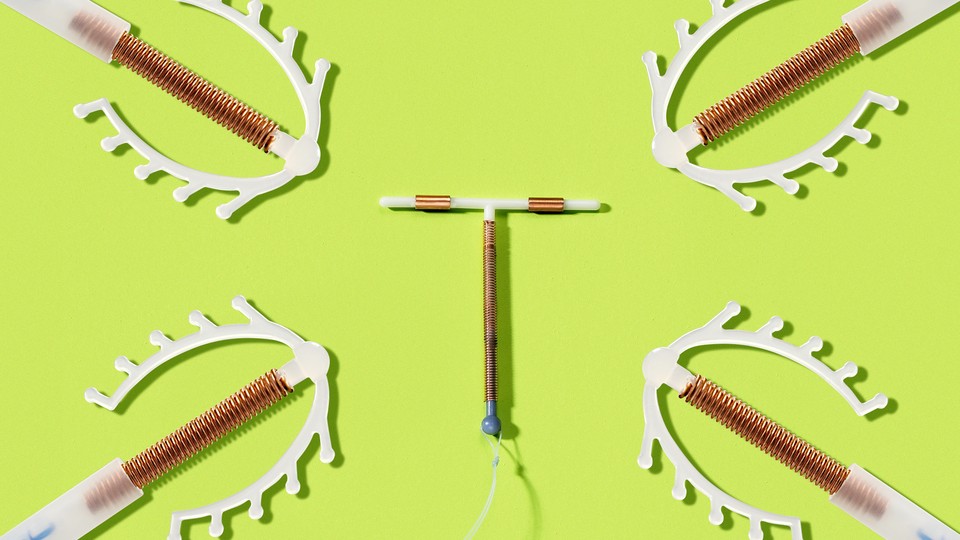
Countries around the world accommodate women’s biological variations and personal preferences with IUDs of different mechanisms, designs, sizes and costs. There are IUDs shaped like balls, loops, omegas, and snakes, and ones made with steel, gold, and even anti-inflammatory drugs. In Britain, there are 22 types of IUDs available, including several short variations for women like me. In Canada, there are nine.
But not in America. In the U.S., there are only five types of IUDs, all with the same T-shape: four hormone-releasing IUDs, which vary only in their size and how much hormone they emit daily, and the copper ParaGard, which has been on the market since 1988. Though the American College of Obstetrics and Gynecologists regards long-acting reversible contraception like IUDs as the gold standard of birth control, America’s IUD options lag far behind other countries’.
* * *
The prevailing explanation for the U.S.’s limited number of IUDs is the Dalkon Shield. In the early 1970s, before the FDA regulated medical devices, this plastic, beetle-shaped IUD caused thousands of injuries including infections, infertility, and even death. Americans filed 300,000 lawsuits–the largest product liability case since asbestos–against and bankrupted the manufacturer, A.H. Robins Company. After the Dalkon Shield, market demand for IUDs died. In the 1980s, contraception innovation nearly halted, and the manufacturers of four of America’s five remaining IUDs pulled their products from the market. Some think that, nearly 50 years later, the Dalkon Shield explains why still just one-in-ten American women use IUDs, compared to several times that many in Europe and Asia.
But there was another side effect of the Dalkon Shield. In 1976, it catalyzed legislation authorizing the FDA to regulate medical devices ranging from pacemakers to IUDs. It also gave the FDA “virtually unlimited discretion” to decide how devices were classified. So, crucially, the FDA decided to regulate IUDs with active substances such as metals and hormones as drugs, rather than devices. Since drugs are more stringently regulated, “the 1976 decision was a stopgap way to put IUDs through the existing rigorous drug approval process given what happened [with the Dalkon Shield],” explains David Hubacher, a senior epidemiologist at the human development nonprofit FHI 360.
Classifying copper IUDs, which are a simple combination of copper coils and plastic, as drugs is a stretch. The FDA argues that the natural element named copper acts as a drug because it boosts contraceptive efficacy. But barely. IUDs made with just plastic prevent pregnancy 98 percent of the time. Copper and hormone IUDs prevent it more than 99 percent of the time. (For reference, the pill is 91 percent effective with typical use.)
The FDA understandably wants to prevent another Dalkon Shield tragedy, but regulating IUDs as drugs means a longer application and approval process and fewer contraception options for American women.
Whereas devices take three-to-seven years to bring from concept to market and generally don’t require clinical trials, drug approval is more lengthy, costly and rigorous. New drugs take an average of 12 years to hit the market in the United States. So to get a new IUD approved, “you have to do research with thousands of women and follow them over time to measure safety and efficacy,” says Hubacher. Even though the FDA knows that copper and the hormone progestin in IUDs are highly effective and safe, “they still want you to prove it every time,” says John Ziemniak, who works with Wildemeersch as the president of Gwynedd Pharmaceutical Consulting. In other words, even if nothing is different about a new IUD’s active substances, which are known to be safe, the FDA requires exhaustive research before manufacturers can even begin to test a new design.
Some drugs—in fact, one-third of them recently approved by the FDA—get short cuts. If a product is considered life-saving, a breakthrough, or without good alternatives, it can get a truncated approval process and/or an expedited review.
IUDs don’t qualify for these priority approvals, though they serve a vital function. Today, almost half of U.S. pregnancies are unintended—compared to just a third of pregnancies in France, where IUD use is three-times higher. Decades of research show that contraception helps women stay in school, advance their careers, avoid abortions, and get out of poverty. It reduces the gender wage gap, and controls population growth. “When women can choose the [contraceptive] method that’s best for them,” says David Eisenberg, an associate professor of OB/GYN at Washington University in St. Louis, “they will have better, healthier lives, and so will their families.” But because IUDs don’t directly save lives, they’re stuck behind the FDA’s red tape.
In Europe, “they have a 180-degree different approval process,” says Diana DeGette, a Democratic representative from Colorado. European agencies impose fewer regulatory hurdles on new products, and then “they do a really robust post-market review. If they have problems, they call [the drugs or devices] off the market.”
This approach has proven sufficient for IUDs. “There are many types of IUDs in Europe that have been on the market for 20, 30, 40 years,” says Hubacher. “These products are safe and effective.” Half a million women have used the GyneFix in its 12-year lifespan, and Belgium’s regulatory agency has never had to pull an IUD from the market. Likewise, the Liberté IUD has been selling in Canada for five years and in Europe for 19 without a problem, says William Carter, the president of Liberté's Canadian supplier.
These IUDs and many others haven’t even tried to get approval in America.
Carter, who calls the FDA “retentive,” says that the Liberté hasn’t applied for FDA approval because it’s “too much paperwork, too much expense, and too much uncertainty.” It’s not worth it, he says. Carter says he knows of other IUD companies that are attempting approval and “banging their heads against the wall.”
GyneFix’s manufacturer can’t afford the 10 to 15 million dollars it would require to run a U.S.-based clinical trial that would meet the FDA’s standards. Wildemeersch, who has spent his career researching and developing viable IUD options for women worldwide, told me that this is his greatest frustration. Mona Lisa N.V., a company that makes several popular IUDs in Europe, has the same problem. They seriously considered trying to get their IUDs approved in the U.S. but stopped due to the “immense costs,” says Elisabeth Adomaitis, who directs the company’s marketing and product expansion.
Rigid regulations and cost-prohibitive clinical trial requirements—among other factors, like dwindling patents and pricey product liability insurance—sap the profitability of new products and reduce market incentive for smaller manufacturers.
Meanwhile, incumbent IUD manufacturers enjoy a virtual monopoly. “The FDA as it is right now is a huge barrier to entry into that market, and the big drug companies like that just fine,” says Michael Cannon, the director of health policy studies at the CATO Institute, a libertarian think tank. If regulations were less stringent, there would be more drug companies making and marketing more IUDs. And IUDs would be cheaper. Without competition, the manufacturers set the price. The Liberté, which is nearly identical to America’s ParaGard IUD, sells for $52 Canadian. “How in the world is the ParaGard selling for $480-to-$600 dollars in the U.S.?” Carter asks.
* * *
The United Nations’ General Assembly has committed to “universal access to sexual and reproductive health-care services … and the integration of reproductive health into national strategies and programs” worldwide by 2030. Americans, on the other hand, are still undecided.
Part of President Trump’s plan for his first 100 days in office was to fully repeal and replace the Affordable Care Act (ACA). This could mean scrapping the provision mandating insurers to cover all 18 methods of FDA-approved contraception without a copay. Then, insurers could choose not to cover or to only partially cover IUDs because of the upfront cost (though in the long term, they are significantly less costly than any other contraceptive method).
This possibility explains why, when Trump was elected, Planned Parenthood saw a 900-percent increase in patients seeking IUDs, and the number of women visiting their doctors about IUDs climbed nearly 19 percent. According to Cindy Pearson, the executive director of the National Women’s Health Network, women’s reaction of “Oh shit, I’ve got to get an IUD” was driven by logic.
But, in March, House Republican leaders abandoned their proposed replacement of the ACA, the American Health Care Act, knowing it wouldn’t pass a House vote. So the ACA and its contraception-insurance provisions currently remain intact, though the GOP plans to try again with a new, modified replacement plan in May. Congresswoman DeGette, who helped write the gender-equity, contraception-coverage, and family-planning provisions in the ACA, ultimately doesn’t think the GOP will succeed in repealing it. But “we have to stop having these ridiculous debates in Washington about whether we should cover family planning,” she says. “I think we should just establish as a given that it’s a good public policy.” For example, when Colorado offered free IUDs and other long-acting reversible contraceptives to low-income women for six years, it almost halved its abortion and teen-pregnancy rates and saved the state millions of dollars.
But while Trump’s policy proposals don’t bode well for IUD access from an insurance perspective, his promise to strip FDA regulation processes by 75-to-80 percent could theoretically clear the way for the approval of new and more affordable IUDs. But Cannon, of the CATO Institute, doesn’t think a shortened FDA approval process would last. Even if we get a “crusading FDA commissioner” or Congress approves more lenient regulations, Cannon explains, “all it takes is just one harmful drug getting through and one group of patients getting harmed, and the pendulum swings right back.”
It’s possible to change the FDA, however, without deregulating it. As Trump’s FDA commissioner nominee Scott Gottlieb said recently, “there are ways to modernize clinical studies without sacrificing the gold standard” of safety.
For example, while the FDA does technically accept foreign clinical data for new drug applications as long as the studies adhere to U.S. guidelines, foreign IUD manufacturers say that, in practice, clinical trials often have to be re-done in the U.S. at significant length and expense.
Washington University’s Eisenberg says he would trust the findings of research done in countries with similar standard operating procedures to the U.S., like many in Europe. “I do think there could be reciprocity between the FDA and the European drug regulatory agencies,” he says. Hubacher, too, feels that there should be ways to “shorten the path to approval for some products that have a long track record of safety and efficacy in European countries, where the oversight and systems are very good.”
The 21st Century Cures Act, signed in December 2016, allows the FDA to consider such “real world evidence” for some breakthrough drugs and devices. While IUDs probably won’t catch a break under this law because they’re not new, this is a step toward a less burdensome approval process.
For now, America’s contraception options haven’t changed much from 50 years ago. “If you wish, you can make an appointment for GyneFix insertion,” Wildemeersch wrote me from Belgium, a 12-hour flight, three-hour layover, and two trains away. My uterus is stumped.